SHREVEPORT, La. — When Robert Smith met his future girlfriend in 2010, he wanted to take things slowly. For Smith, no relationship had been easy in the years since he was diagnosed with the human immunodeficiency virus, or HIV. People often became afraid when they learned his status, even running away when he coughed.
The couple waited months to have sex until Smith felt he could share his medical status. To prepare her, Smith said, he took his girlfriend to his job in HIV prevention at the Philadelphia Center, a northwestern Louisiana nonprofit that offers resources to people with HIV, which also provided him housing at the time.
Finally, he revealed the news: Smith was diagnosed with HIV in 1994 and started taking daily antiviral pills in 2006. The virus could no longer be detected in his blood, and he couldn’t transmit it to a sexual partner.
Smith said his girlfriend seemed comfortable knowing his status. When it came to sex, there was no hesitation, he said. But a couple of years later, when Smith wanted to break up, he said, her tone shifted.
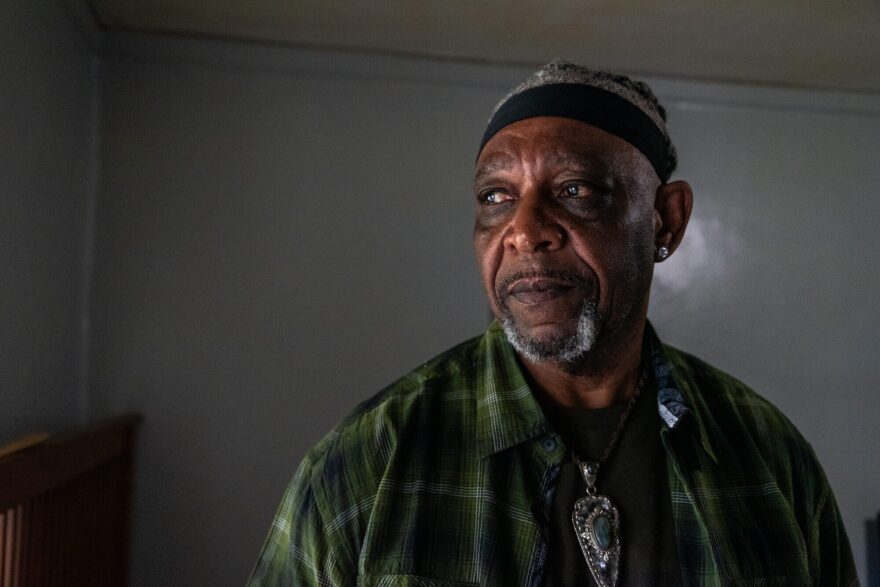
“She was like, ‘If you try to leave me, I’m gonna put you in jail,’” recalled Smith, now 68. “At the time, I really didn’t know the sincerity of it.”
After they broke up, she reported him to the police, accusing him of violating a little-known law in Louisiana — a felony called “intentional exposure to HIV.” He disputed the allegations, but in 2013 accepted a plea deal to spend six months in prison on the charge. He had a few months left on parole from a past conviction on different charges, and Smith thought this option would let him move past the relationship faster. He didn’t realize the conviction would also land him on the state’s sex offender registry.
For nearly two decades, Smith had dealt with the stigma associated with having HIV; the registry added another layer of exclusion, severely restricting where he could live and work to avoid minors. Not many people want to hire a sex offender, he said. Smith has been told by the local sheriff’s office he’s not allowed to do simple things, like go to a public park or a high school football game, since the conviction.
“I’ve been undetectable for 15 years, but that law still punishes us,” Smith said.
Louisiana is one of 30 states with criminal penalties related to exposing or transmitting HIV. Most of the laws were passed in the 1980s during the emergence of the AIDS epidemic. Since then, several states have amended their laws to make them less punitive or repealed them outright, including Maryland and North Dakota this year.
But Louisiana’s law remains among the harshest. The state is one of five that may require people such as Smith to register as a sex offender if convicted, a label that can follow them for over a decade. And state lawmakers considered a bill to expand the law to apply to other sexually transmitted infections, then failed to pass it before the session ended.

Meanwhile, people with HIV also face the threat that federal funding cuts will affect their access to treatment, along with prevention efforts, supportive services, and outreach. Such strategies have proved to slow the HIV/AIDS epidemic, unlike the laws’ punitive approach.
The tax and domestic policy law previously known as the “One Big Beautiful Bill” will likely affect HIV-positive people enrolled in Medicaid by reducing federal support for Medicaid and restricting eligibility. About 40% of adults under 65 with HIV rely on Medicaid.
The Trump administration proposed in its fiscal 2026 budget request to eliminate HIV prevention programs at the Centers for Disease Control and Prevention and to cancel a grant that helps fund housing for people with HIV. The Ryan White HIV/AIDS program, the largest federal fund dedicated to supporting HIV-positive people, also faces cuts. The program serves more than half of the people in the U.S. diagnosed with HIV, including in Louisiana, according to the health information nonprofit KFF.
Public health officials maintain that state laws criminalizing HIV exposure hurt efforts to end the HIV epidemic. Epidemiologists and other experts on AIDS agree that the enforcement of such laws is often shaped by fear, not science. For example, in many states that criminalize HIV exposure, people living with HIV can face heightened criminal penalties for actions that can’t transmit the virus, such as spitting on someone. The laws further stigmatize and deter people from getting tested and treatment, undermining response to the epidemic, experts say.
At least 4,400 people in 14 states have been arrested under these laws, though data is limited and the actual number is likely higher, and the arrests aren’t decreasing, according to analyses by UCLA’s Williams Institute.
“ Some people think it’s an issue that’s gone away, and that simply isn’t the case,” said Nathan Cisneros, a researcher at the Williams Institute.
In Louisiana, a 2022 Williams Institute analysis found at least 147 allegations reported to law enforcement under the state’s HIV law from 2011 to mid-2022. Black people made up nearly three-quarters of the people convicted and placed on the sex offender registry. Most were Black men, like Smith. At the time of the analysis, Black people made up about two-thirds of HIV diagnoses in the state.
“ We see over and over that Black people are disproportionately affected by the HIV epidemic and disproportionately affected by policing and incarceration in the United States,” Cisneros said.
Nationally, other marginalized groups such as women, sex workers, the queer community, or people who overlap across more than one group are also disproportionately arrested and prosecuted under similar criminalization laws, Cisneros said.
Ensnared in the system
Louisiana’s law hinges on the requirement that if a person knows they have HIV, they must disclose their HIV status and receive consent before exposing someone to the virus.
Louisiana District Attorneys Association Executive Director Zach Daniels said these cases don’t come up often and can be difficult to prosecute. Daniels said the intimate nature of the cases can lead to little evidence in support of either side, especially if the accuser doesn’t contract HIV.
When it comes to talking about one’s sex life, Daniels said, “there are often no other witnesses, besides the two participants.”
Louisiana’s law is written so that “intentional exposure” can occur through “any means or contact.” That includes sex and needle-sharing, practices known to transmit the virus. But the language of the law is so broad that actions known not to transmit the virus — like biting or scratching — could be included, said Dietz, the statewide coordinator for the Louisiana Coalition on Criminalization and Health, an advocacy network founded by people living with HIV that has opposed the law.
The broad nature of the law creates opportunities for abuse, as the threat of being reported under the law can be used as a coercive tool in relationships, said Dietz, who goes by one name and uses they/them pronouns. Such threats, Dietz said, have kept people in abusive relationships and loomed over child custody battles. Dietz said they’ve supported people accused of exposing their children to HIV in ways that are not medically possible.
“ ‘Any means or contact’ could be just merely being around your kids,” they said.
The prosecutors’ organization still supports the law as a recourse for emergency responders who, in rare instances, come into contact with blood or syringes containing the virus. In one recent high-profile case in New Orleans, the law was used against a local DJ accused of knowingly transmitting HIV to several women without informing them of his status or using a condom.
The person accused of violating the law, not the accuser, must prove their case — that they disclosed their HIV status beforehand. Without a signed affidavit or tape recording, courts can end up basing their decisions on conflicting testimonies with little supporting evidence.

That’s what Smith alleged happened to him.
After his relationship ended, he said, he remembered being called into a meeting with his parole officer where a detective waited for him, asking about his former relationship and whether his girlfriend had known about his HIV status.
Smith said yes. But that’s not what she had told police.
Verite News could not find a working phone number for Smith’s former girlfriend but corroborated the story with the incident’s police report. His attorney at the time, a public defender named Carlos Prudhomme, said he didn’t remember much about the case, and court documents are sealed because it was a sex offense.
In court, it was her word against his. So when he was offered six months in prison instead of the 10-year maximum, he switched his plea from not guilty to guilty. But he said he didn’t know his new conviction would require him to register as a sex offender once he got out — worsening the stigma.
“When people see ‘sex offender,’ the first thing that comes to their mind is rape, child molester, predator,” Smith said. “This law puts me in a category that I don’t care to be in.”
He has tried to make the most of it, despite the expense of paying fees each year to re-register. After being rejected from jobs, he started a catering business and built a loyal clientele. But he said he’s still stuck living in a poorly maintained apartment complex primarily inhabited by sex offenders.
“I understand their strategy for creating this law to prevent the spread, but it’s not helping. It’s hurting; it’s hindering. It’s destroying people’s lives instead of helping people’s lives, especially the HIV community,” he said. “They don’t care about us.”
The case for reform
Since 2014, there has been a nationwide effort to update or repeal state laws that criminalize HIV nondisclosure, exposure, or transmission. A dozen states have changed their laws to align more closely with modern science, and four have gotten rid of them completely in hopes of reducing stigma and improving public health outcomes, according to the Center for HIV Law and Policy.
Sean McCormick, an attorney with the center, said these changes are influenced partly by a growing body of evidence showing the laws’ negative consequences.
McCormick said the laws offer a “clear disincentive” for people to get tested for HIV. If they don’t know their status, there’s no criminal liability for transmission or exposure.
A 2024 survey by Centers for Disease Control and Prevention and DLH Corp. researchers found that after California updated its HIV criminalization law in 2018, respondents were more likely to get tested. Meanwhile, survey respondents in Nevada, which still had a more punitive law on the books, were less likely to get tested.
There’s no one-size-fits-all solution, McCormick said. His center works with HIV-positive people across the country to determine what legislative changes would work best in their states.
Texas was the first to repeal its HIV law in 1994.
“As a person living with HIV in Texas, I’m deeply appreciative that we don’t have an HIV-specific statute that puts a target on my back,” said Michael Elizabeth, the public health policy director for the Equality Federation.
But Elizabeth points out that Texans living with HIV still face steeper penalties under general felony laws for charges such as aggravated assault or aggravated sexual assault after state courts in Texas equated the bodily fluids of a person with HIV with a “deadly weapon.”
Louisiana activists have pushed lawmakers in the state to amend the law in three ways: removing the sex offender registration requirement, requiring transmission to have occurred, and requiring clear intent to transmit the virus.
“Our strategy, as opposed to repeal, is to create a law that actually addresses the kind of boogeyman that they ostensibly created the law for: the person who successfully, maliciously, intentionally transmits HIV,” said Dietz with the Louisiana Coalition on Criminalization and Health.
In 2018, a bill to narrow the statute was amended in ways that expanded the law. For example, the updated law no longer had any definition of which actions “expose” someone to HIV.
In 2023, state lawmakers created a task force that recommended updating Louisiana’s law to align with the latest public health guidelines, limit the potential for unintended consequences, and give previously convicted people a way to clear their record.
Lawmakers in the state House pushed forward a bill this year to criminalize other sexually transmitted infections, including hepatitis B and the herpes simplex virus. That bill died in the Senate, but it spurred the creation of another legislative task force with a nearly identical mission to that of the first.
“ This state has no idea how closely we just dodged a bullet,” Dietz said.

In the meantime, the Louisiana coalition is helping Smith petition the state to take his name off the sex offender registry. Louisiana law allows people to petition to have their names removed from the registry after 10 years without any new sex crime convictions. Smith expects his case to be approved by the end of the year.
Despite the difficulty of the past 12 years, he said, he’s grateful for the chance to be free from the registry’s restrictions.
“It’s like a breath of fresh air,” Smith said. “I can do stuff that I wanted to do that I couldn’t. Like, go to a football game. Simple stuff like that, I’m going to be ready to do.”
This story was produced in collaboration with KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.